May 22nd, 2020
“The only way to avoid ‘groupthink’ and blind spots is to ensure representatives with diverse backgrounds and expertise are at the table when major decisions are made.”
Devi Sridhar, Chair of Global Health at the University of Edinburgh Medical School
Bolivia is an amazingly diverse and heterogeneous country in every way. Within a million square kilometers we find both steamy Amazon jungle, large modern cities, mosquito infested swamps, melting glaciers, huge salt flats, and picturesque cloud forests. Some people live pretty much as their ancestors did hundreds of years ago, while others enjoy all the luxuries of the most advanced countries. According to our upcoming Municipal Atlas of the SDGs in Bolivia, the differences between municipalities within Bolivia are larger than the differences between all the countries in the world in terms of the Sustainable Development Index (SDI). And as within countries, there are also large inequalities within each municipality in Bolivia.
In this blog, I will argue that we should take advantage of this heterogeneity to reduce the mortality rate of COVID-19 in Bolivia.
Good News of the Week
About a month ago, the World Health Organization (WHO) came out with a worrying statement saying that “there is currently no evidence that people who have recovered from COVID-19 and have antibodies are protected from a second infection” [1]. If this were true, it would be very bad news for the many countries, including Bolivia and its neighbors, that have failed at containing the virus, have no test-trace-and-quarantine capacity, and whose only option to get through this pandemic therefore is to achieve herd immunity.
The good news out of the Korean Center for Disease Control (KCDC) last week was that the 263 people in Korea who tested positive for the disease a second time after previously being declared recovered and virus-free, was not due to re-infection nor re-activation of the SARS-CoV-2 virus. Rather, it was due to the PCR tests picking up old, inactive, and harmless virus RNA still present in the body a couple of months after the original infection. According to KCDC, the process in which COVID-19 produces a new virus takes place only in the cytoplasm of the host cells and does not infiltrate the nucleus. This means it does not cause chronic infection or recurrence, unlike viruses like HIV [2].
Thus, it seems that the herd immunity strategy might be viable after all. Once 60-70% of the population has become immune, the virus will die out, as it becomes difficult for it to find new hosts in which to multiply. The question now is how to apply that strategy with the least number of deaths and collateral damage possible.
Optimizing the Herd Immunity Strategy
I previously estimated that we will likely “end up with an Infection Fatality Rate (IFR) of around 1% for Bolivia (meaning anywhere between 0.3% and 2%, given the still high uncertainty). If 60% of 11.6 million people get infected, and 1% of those die, we would end up with about 70 thousand COVID-19 deaths in Bolivia” [3]. While this is an awful lot of deaths, the 1% IFR is a realistic estimate considering the age distribution of the population, underlying health conditions, the quality of the health care system, typical housing and work conditions, in addition to the level of education and trust in the population. It looks like the most likely outcome if we let the virus burn slowly through the population (through appropriate physical distancing measures) in a random way until reaching herd immunity after 12-18 months, and if we don’t actively make things worse than they have to be.
However, the IFR can be lowered considerably if we take advantage of the fact that the population is not homogeneous. Some people have far lower risk of dying from COVID-19 than others, so if we could secure that the first 60% to get infected are the ones least likely to suffer severe complications, then we could potentially reduce the total number of deaths considerably.
In the rest of this blog I will outline the main dimensions to consider when optimizing the herd immunity strategy.
1. The Demographic Dimension
The evidence from all over the world shows unequivocally that the risk of death from COVID-19 is higher in older people. In Italy, for example, until May 18th, only 4 people under 20 years of age had died, while the number of deaths of people over the age of 50 was almost 30,000 (see Figure 1).
Figure 1: COVID-19 deaths in Italy as of May 18, 2020, by age group
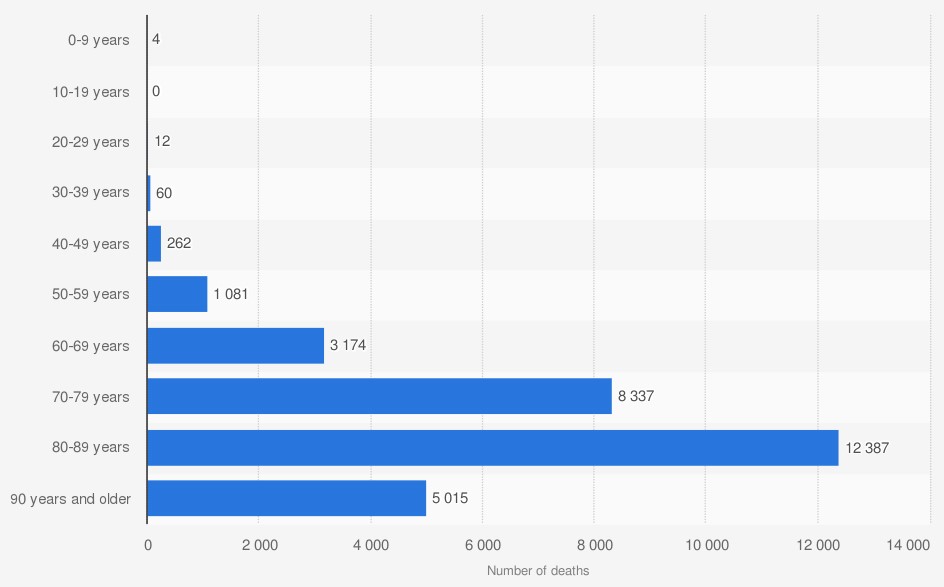
Source: Istituto Superiore di Sanità (via Statista 2020).
There is also overwhelming evidence that men are almost twice as likely to die from COVID-19 compared to women. Figure 2 shows the case fatality rates observed in Italy to date, disaggregated by age and gender.
Figure 2: COVID-19 death rates in Italy as of May 2020, by gender and age group
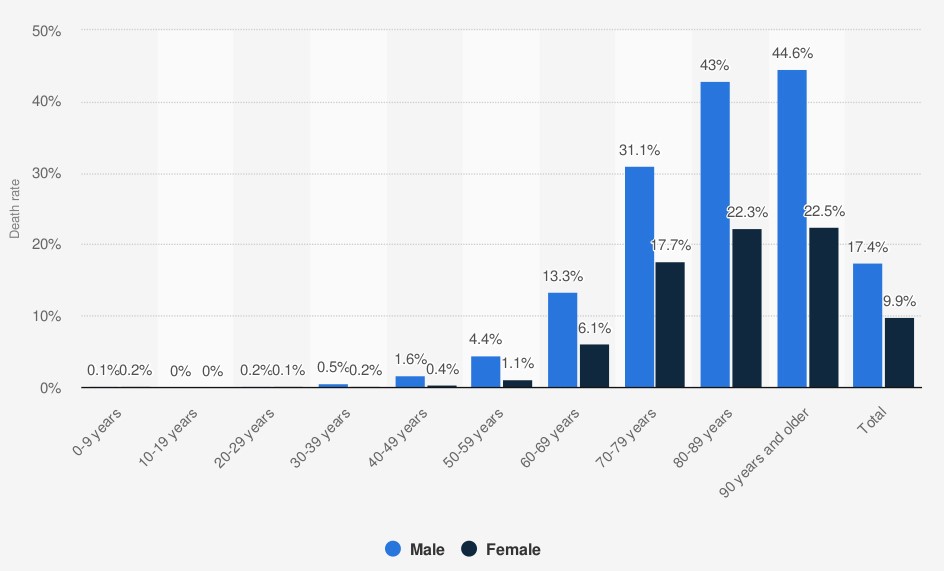
Note: The case fatality rates in this figure do not reflect the real Infection Fatality Rates, as there are errors
in both the nominator (un-counted COVID-19 deaths) and denominator (un-identified COVID-19 cases).
However, the overall pattern by age and gender is likely to reflect the actual differences in IFRs by age and gender.
Source: Istituto Superiore di Sanità (via Statista 2020).
Given this pattern, and similar patterns from all other countries with age and gender disaggregated COVID-19 death statistics, we can make the following rough demographic risk classification:
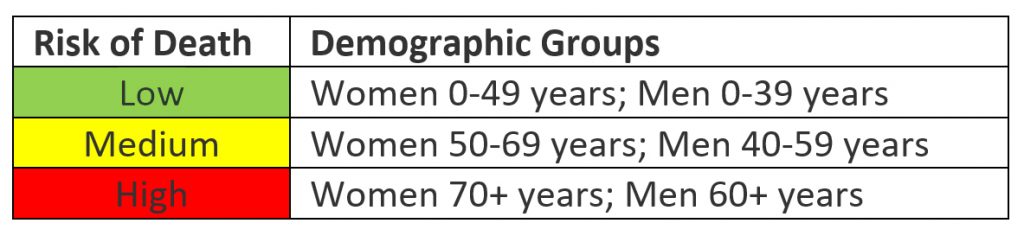
If we apply this classification to the population pyramid of Bolivia, it looks as shown in Figure 3.
Figure 3: Population Pyramid for Bolivia, with risk categories
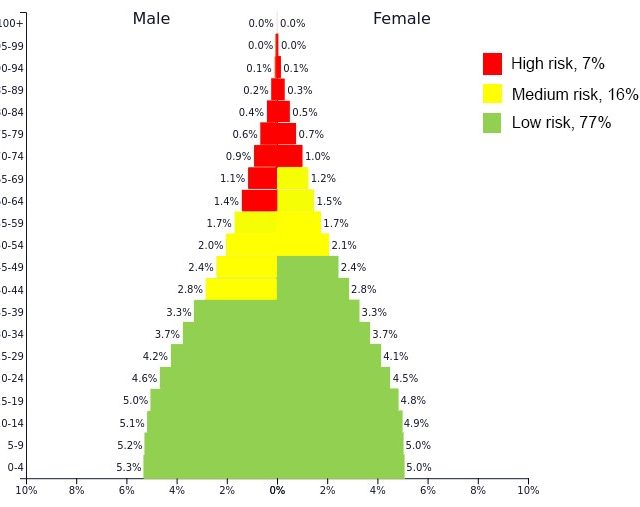
Source: Author´s elaboration based on data from PopulationPyramid.net
Based on just these basic demographic factors, 77% of the Bolivian population is at Low Risk of dying if contracting COVID-19; 16% is at Medium Risk; and 7% is of High Risk.
But there are more risk dimensions to take into consideration.
2. The Geographic Dimension
While age and gender are important determinants of risk, there are factors in the surrounding community that can either amplify or moderate the risk for each individual.
- It is safer to live in a disperse rural area where you interact with few different people, than to live in a dense urban area touching public surfaces that thousands of other people touch every day.
- It is safer to live alone, rather than in a three-generation extended household.
- It is safer to live in a place that is not simultaneously plagued by other health threats, such as Dengue, Malaria, Tuberculosis and HIV.
- It is safer to live in an area where there are basic water and sanitation services available.
In last week’s blog we developed a Municipal Vulnerability Index to COVID-19 [4], and while it is a continuous indicator, we can roughly divide it into Low, Medium and High Risk municipalities, with some admittedly arbitrary cut-offs. If we consider all municipalities with a Vulnerability Index higher than 36.7 High Risk, and lower than 31.7 Low Risk, then we get a municipal risk list as shown in Figure 4.
Figure 4: Municipal level COVID-19 Vulnerability Index, with risk categories.
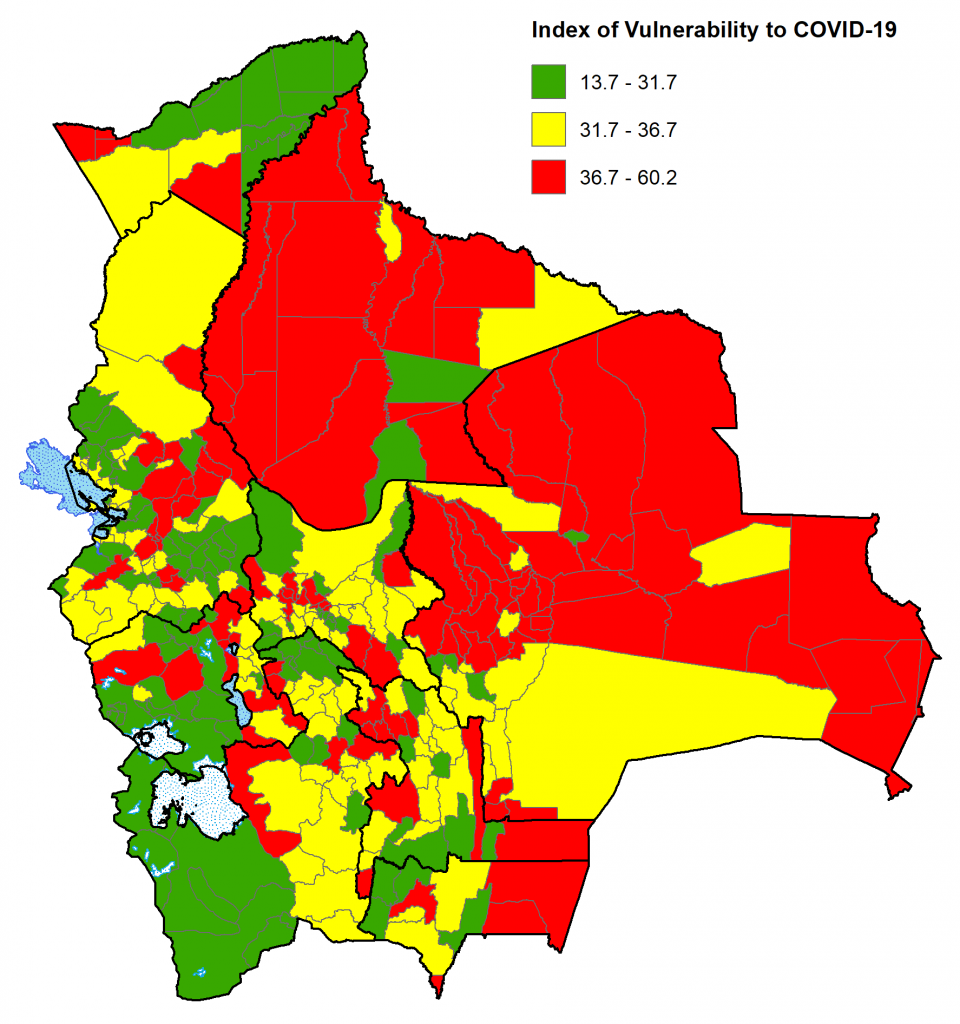
(Click here to see details)
Source: Between a Wall and a Nasty Virus [4].
This Vulnerability Index only considers structural variables, and not actual infection rates, which would also be important to consider, but these suffer daily changes, and due to the limited testing capacity, many cases go undetected.
3. Occupational Dimension
Even for people of the same age and gender, living in the same municipality, risk will vary substantially depending on the kind of activities each of them engages in. The risk will be extremely high if you work as a dentist, but extremely low if you collect Brazil nuts alone in the forest.
In general, solitary outdoor activities are much safer than working indoors with lots of different people cramped together. The highest risk occupations would be those where you must be very close to many different, potentially infected people every day, such as dentists, doctors, and nurses. If you work at, or frequent, indoor locations where people are singing, screaming or breathing heavily, such as night clubs, karaoke places, churches, and gyms, you are also at high risk, as the virus spreads very effectively in this kind of places.
4. Individual Risk Factors
Apart from all the above mentioned risk variations, there will be additional personal risks that can be either permanent or temporary. For example, anyone who suffers from high blood pressure, diabetes or asthma would automatically and permanently move to a higher risk category than the one suggested by their age, gender, location, and occupation.
Likewise, anybody who presents COVID-19-like symptoms, irrespective of their age, gender, location, and occupation, should immediately consider themselves at High Risk and take every precaution to protect themselves and others.
Individual risk factors should also take into account other people in the same household. One individual might be young and healthy, but if they live together with a High Risk person, their risk category increases, because their actions might carry risks not to themselves, but to their loved ones.
Central Planning is Unlikely to Work
From the analysis above it is obvious that risks vary by several orders of magnitude from place to place and from person to person. This makes centralized decisions extremely difficult, and uniform rules will likely be both inefficient and harmful.
The initial strict quarantine measures have served to educate people about the dangers of this virus and about the hand-washing and physical distancing measures that can help control contagion. But these strict measures are clearly not sustainable over the many months that this pandemic is likely to last [5], and it is time for a more nuanced approach.
Decentralization of Decisions and Responsibilities
If our goal is to reach herd immunity with the least number of deaths and collateral damage possible, then we need to decentralize decisions considerably. Each department, each municipality, each business, each school, and each family need to analyze their strengths and weaknesses in this new global context, and make a plan on how to get through the following 24 months with the slightest possible damage. Damage not only includes COVID-19 deaths, but also loss of education, income, freedom, agency, joy, and happiness; so everybody needs to engage in quite a holistic analysis, which is not easy. It will take patience, communication, collaboration, and many iterations.
The need for decentralization of decisions and responsibilities is even greater now that the central government is facing a precipitous decline in revenues from all sources (especially IDH, IVA, IT, IUE, ICE, and RC-IVA), and thus will have much fewer funds available for distribution to departments, municipalities, and individuals.
We need to recognize that there are no right answers. Nobody knows the best way to get through this, and there is no one-size-fits-all solution. Nobody knows what the world is going to look like on the other side. This is a good time to be flexible, think out-of-the-box, and try out new ways of learning, working, and living.
Learning quickly is more important than ever, and learning is only possible if we try different strategies and learn from their different results. The best way to do that is to let municipalities pursue different strategies and record results more or less in real time.
The Need for Timely, Geographically Disaggregated Data on Deaths from All Causes
Since we have extremely limited testing capacity all over the world, and especially in Bolivia, reported COVID-19 cases and deaths rarely reflect reality. It is more feasible and useful to simply register the total number of deaths (by age and gender) per week from all causes, and compare that to the expected number of deaths per week in each territory.
According to INE, we expected 66,760 deaths in Bolivia this year without the COVID-19 pandemic [6], corresponding to 1,284 deaths per week in the whole country. This data can be disaggregated to the department level by applying the departmental crude deaths rates calculated by INE to the population of each department (see Table 1).
Table 1: Expected weekly deaths, 2020, by department
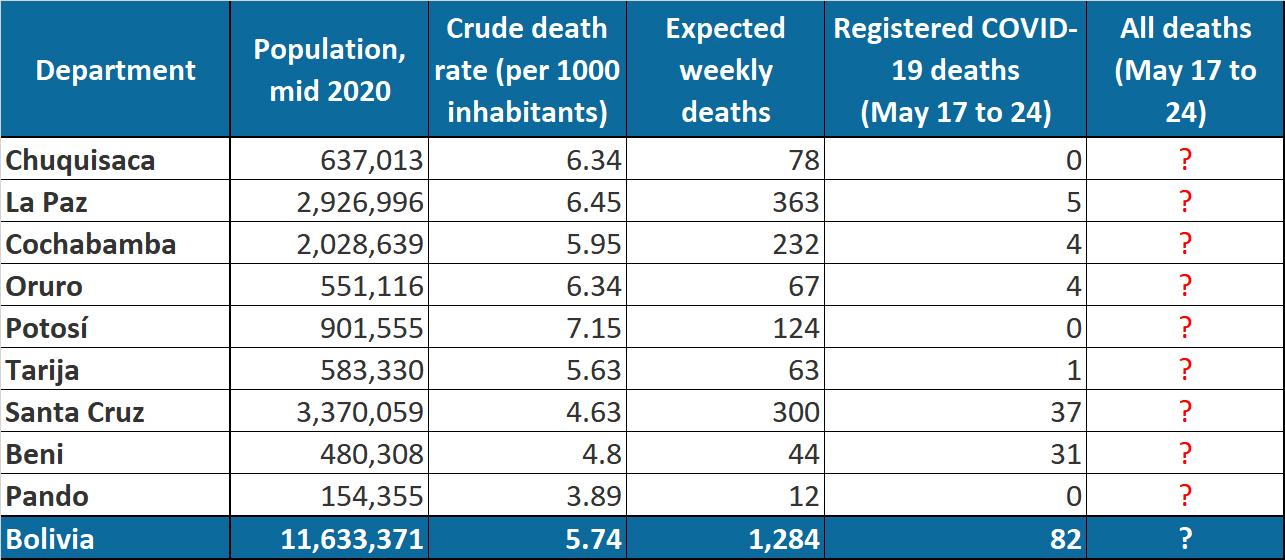
Source: INE and https://www.covid19bo.com/
According to this data, Beni is the only department in Bolivia that has a serious COVID-19 outbreak at the moment, probably because it is particularly vulnerable to a COVID-19 outbreak (due to high levels of obesity, low coverage of water and sanitation, crowded housing, simultaneous Dengue, Malaria, Tuberculosis, and HIV outbreaks, and low local government capacity), as we showed in our blog a couple of weeks ago [4]. However, the real number of COVID-19 deaths is likely far higher, since only people with a positive COVID-19 tests are counted. The dedicated COVID-19 cemetery in Trinidad (Beni), for example, a few days ago held 148 deceased, of which only 57 were confirmed COVID-19 deaths, while 91 were suspected [7].
In the table above, there are question marks in the last column concerning the number of deaths from all causes. This information is currently not available from any government entity in Bolivia. My recommendation to the National Statistical Institute of Bolivia (INE) would be to quickly build up a system to record number of deaths in each municipality each week by age and gender.
Weekly, geographically disaggregated information on all deaths by age and gender is necessary to carefully monitor local outbreaks and take adequate precautions in the right places [8].. A fine-tuned, decentralized response to this pandemic, requires timely disaggregated data. It is well worth the effort to set up the information gathering and reporting system, as it can save tens of thousands of lives and avoid a lot of unnecessary economic costs and human suffering.
—-
Footnotes:
[1] https://time.com/5827450/who-coronavirus-antibodies-reinfection/
[2] http://m.koreaherald.com/view.php?ud=20200429000724. See John Campbell’s video for an easy-to-understand interpretation of the findings: https://www.youtube.com/watch?v=uATMbGK__Tg&t=1200s. See MedCram for a much more detailed, intracellular, explanation of the same thing: https://www.youtube.com/watch?v=01Rftnxbi6w.
[3] https://www.sdsnbolivia.org/en/english-forty-days-of-quarantine-what-have-we-learned/
[4] https://www.sdsnbolivia.org/en/entre-la-pared-y-un-terrible-virus/
[5] The World is still in the very early phases of this pandemic, with even hard-hit countries still having a long way to go before reaching herd immunity. By early May, it was estimated that Belgium was the country closest to herd immunity, with 6.4% of the population having been infected, while in other European countries the immune population is still less than 5%. In certain hot-spots, like Madrid, the rate is much higher, but still nowhere near immunity (https://www.ft.com/content/f7d08906-b5c5-4210-b2c6-0ec95d533bc6).
[6] https://www.ine.gob.bo/index.php/censos-y-proyecciones-de-poblacion-sociales/#
[7] This page by Our World In Data provides a collection of sites monitoring excess mortality (https://ourworldindata.org/excess-mortality-covid). The Economist, Financial Times, the New York Times and EUROMOMO all provide excellent examples of how this data can be presented in user-friendly ways.
* SDSN Bolivia.
The viewpoints expressed in the blog are the responsibility of the authors and do not reflect the position of their institutions. These posts are part of the project “Municipal Atlas of the SDGs in Bolivia” that is currently carried out by the Sustainable Development Solutions Network (SDSN) in Bolivia.

 Español
Español

